Ashleigh Bergstrom, FNP, shares a story about a patient she cared for who initially enrolled in Palliative Medicine and later transitioned to hospice care. Here’s that patient’s story.
—
One of my first Palliative Medicine patients was a young woman with a glioblastoma. She had actually been working as a nurse when she was initially diagnosed. Over the course of a year, she experienced an unfortunate significant decline despite aggressive therapy with her oncology team.
When I first met the patient, she was struggling with a decision about whether or not to enter hospice care. While she was clearly medically qualified for hospice and, as a nurse, was very aware of her overall poor prognosis, she still desired radiation and several other aggressive therapies. She had a strong desire to hold onto her independence as long as possible, and she felt that these therapies helped improve her function somewhat.
A Desire to Pursue Curative Treatments
Because she still wanted to pursue curative treatments, she decided to enroll in Palliative Medicine. She wanted to have palliative act as a bridge until she was ready to stop those aggressive therapies, which she knew, at some point, she ultimately would.
During her time on palliative care, she experienced many complications, including blood clots. I had multiple conversations with her primary medical team, the patient, and her daughter. The discussions covered symptom management, goals of care, and risk-benefit analysis of each of her various therapy choices. She ultimately chose one final hospitalization, elected IVC filter placement due to the blood clots, and then decided to stop her radiation and cancer therapies and discharge home with hospice care.
The Transition to Hospice Care
Due to her already being on palliative care, the transition to hospice was very smooth.
While receiving palliative care, she and her family had asked many questions in preparation for hospice. So, she wasn’t surprised by anything. By the time she came on hospice, she knew all the details about which medications would be formulary, how medication orders would be processed, how DME would work, how patient visits would work, and who her hospice team would be. Our hospice team was also able to get a little bit of a heads-up prior to her being admitted.
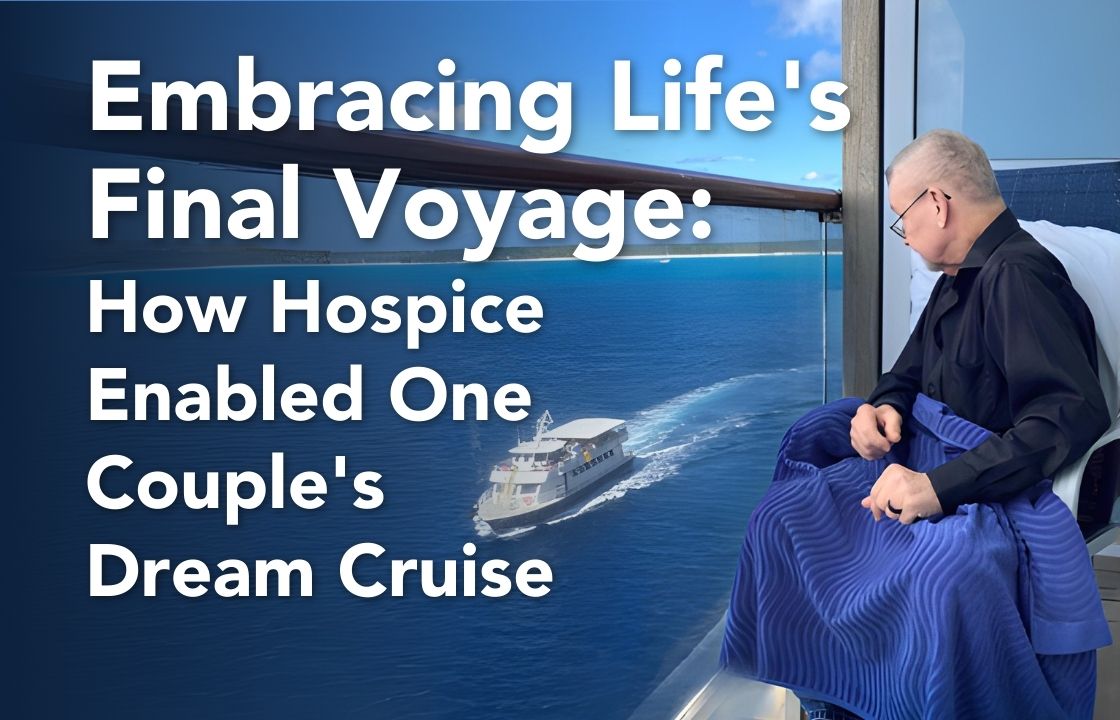
The patient was admitted to an amazing team of people who—unsurprisingly—took excellent care of her. They helped to facilitate medical details for going on a “bucket list” beach vacation with her family. She ultimately died comfortably at home with her family in accordance with her wishes.