Hospice of the Piedmont’s Palliative Medicine program recently celebrated its third anniversary. To mark the occasion, we sat down with our Director of Palliative Medicine, Lara Fisher, to learn how the Palliative Medicine program fits into HOP’s services and why there’s still so much confusion about palliative care vs hospice.
Why create a Palliative Medicine program within a Hospice?
The Palliative Medicine program enrolled its first patient on Christmas Eve 2019, which is a funny coincidence because, in a way, the program was a gift to the community.
“Prior to the launch of Palliative Medicine, if someone called and said, ‘Hey, I want help.’ We’d have to ask, ‘Do you have six months or less to live?’ And, if they said, ‘No,’ unfortunately, there wasn’t much we could do to help that person,” explains Fisher.
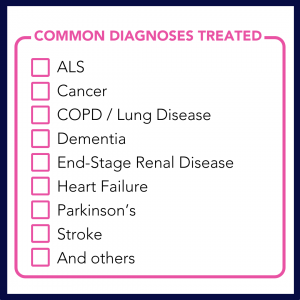
With the Palliative Medicine program up and running, HOP can serve more community members. “Patients are not forced to choose between treatments and receiving the extra support of palliative care,” says Fisher. Some common diagnoses that can benefit from palliative care include ALS, Cancer, COPD, and others (see list).
Palliative Care vs Hospice
So why is there so much confusion between palliative care and hospice? “Well, to start with, I think there’s confusion about each of those individually,” chuckles Fisher.
Many people still erroneously believe hospice is for the last few days of life. “People think you only get on hospice when you’re ready to pull the blankets up to your chin and say goodbye. There are still so many misconceptions about that,” says Fisher.
In some ways, signing up for hospice is a little like ordering a supreme pizza – it comes with everything. Hospice’s team structure includes support from doctors, nurses, home health aides, social workers, and chaplains. Receiving palliative care from doctors and nurses is a key ingredient, but there are lots of other wonderful ingredients, too. And it benefits (feeds, perhaps?) the whole family.
Palliative care is more like ordering a pepperoni pizza. You’re getting one topping, which is still great. And maybe you still have some room left over for salad. And by “salad,” I mean chemotherapy and other aggressive medical treatments. That’s because signing up for a Palliative Medicine program does not preclude patients from pursuing curative therapies.
The point is: palliative care can be enjoyed by itself or with other services. It can be a part of hospice care, or it can be a part of other medical treatments.
What is Palliative Care?
Simply stated, palliative care is comfort care for someone with an advanced illness that treats patients holistically and helps to improve their overall quality of life. As Fisher points out, “I think sometimes people have a hard time understanding palliative because they think, ‘Well, isn’t that just good healthcare?’”
A useful framework for understanding palliative care is to think about two areas where HOP’s Palliative Medicine program provides assistance: Symptom Management and Goals of Care.
Symptom Management
Palliative care helps patients with serious illnesses manage symptoms caused by their underlying disease or side effects from treating that disease. Some of the common symptoms palliative providers help with are:
- Anxiety
- Pain
- Nausea / Vomiting
- Fatigue
- Shortness of breath
- Trouble sleeping
HOP’s team of nurse practitioners can work with a patient’s primary care physician to prescribe medications if that makes sense, or “de-prescribe” medications if necessary. As Fisher points out, “Sometimes you have four different providers who have – all in good faith – given you a medication. Now you have these four medications with side effects. Maybe there are two that you could take that would provide the same benefit without having all those side effects.”
Goals of Care
Goals of care is a term our Palliative Medicine team uses to describe building relationships with patients and gaining alignment among patients, families, and the extended medical team. This area includes four main benefits.
-
Personalized listening at home
Our Nurse Practitioners visit patients in their homes and generally spend more time with a patient than in a typical doctor’s office appointment. “The patient gets to spend time with a Nurse Practitioner who can be a sounding board for their concerns,” says Fisher. “Those NPs can give patients tools to make decisions about their healthcare in a way that doesn’t happen in many other healthcare settings.”
-
Treating the whole person
Seeing patients in their homes helps NPs to observe patients holistically. “They’re seeing a whole picture and assessing their quality of life. They can say, ‘I see you’re having trouble walking your dog to the mailbox. What can we do to make that easier?’” explains Fisher.
-
Coordinating with other providers
The Nurse Practitioners in HOP’s Palliative Medicine program take the time to understand the effect of each specialist a patient sees. “We’re reviewing medical records from every specialty and sending our notes to your primary doctor and your oncologist and your nephrologist,” she explains. “We’re making sure everyone knows what the other specialty is doing. That collaboration is incredibly valuable.”
-
Exploring scenarios
When “battling” a complex illness, having someone who can help a patient understand how a disease might progress is essential. Our team takes time to discuss situations and potential scenarios with patients and their families. “We had a patient come on service, and he didn’t really know all his options,” explains Fisher. “Our NP talked him through it, and he said, ‘The next time I go to the hospital, I’m going to let them know what my decision is.’ He could advocate for himself in a way he couldn’t have previously.”
From Palliative to Hospice and Vice Versa
While palliative care and hospice are different, that doesn’t mean they’re unrelated. Palliative medicine can be a gateway to hospice care, but like any gate, it swings both ways. And sometimes, patients fully recover and no longer need palliative care.
In her sixteen years with Hospice of the Piedmont, Fisher has seen patients with all kinds of perspectives on hospice and palliative medicine. “Some people want to get onto hospice as soon as possible because they know how good the support is. And other people never want to be on hospice care. But then sometimes they hear about what hospice provides and say, ‘Oh, wait, I do want that,’” she laughs.
Of course, not everyone is confused about the difference between hospice and palliative care. Ashleigh Bergstrom, one of HOP’s Palliative Nurse Practitioners, recently wrote about her experience caring for a fellow nurse with a glioblastoma. As a healthcare professional, the patient knew all about hospice and palliative care. She enrolled in the Palliative Medicine program as a bridge to hospice, knowing full well that her time in the palliative program would be temporary.
Yet, sometimes, the gate swings in the other direction. Fisher explains one scenario where a patient experienced a stroke and was admitted to hospice. “The stroke was initially very debilitating. But, as a result of our hospice team’s care, the patient improved. He didn’t return to his total baseline but reached the point where he no longer had a six-month prognosis. So, he was no longer eligible for hospice. That’s when our palliative program could step in and offer support.”
Over the last three years, the Palliative Medicine program has been a valuable addition to the Hospice of the Piedmont by supporting people looking for help but aren’to eligible for hospice care. Visit our Palliative Medicine program page to learn more.